Hip Replacement & Arthritis
Center of Excellence
Rediscover the joy of movement and the freedom to live life on your terms with our expert orthopedic hip replacement expertise. At Orthopedic Centers of Colorado, we understand that hip pain can significantly impact your quality of life, limiting your ability to perform everyday activities and pursue your passions. Our dedicated team of orthopedic specialists is here to provide compassionate care and advanced solutions to help you reclaim your mobility and independence.
Hip replacement surgery, also known as total hip arthroplasty, is a transformative procedure that can relieve pain and restore function for individuals suffering from severe hip arthritis. Orthopedic Centers of Colorado surgeons are leaders in the field, with extensive experience performing hip replacement surgeries using the latest techniques and technologies. Our dedicated team of orthopedic specialists is here to provide compassionate care and comprehensive solutions to help you reclaim your quality of life.
Schedule Now!
Click below to schedule
an appointment
Comprehensive Care
Preoperative Evaluation: Your journey to hip replacement begins with a thorough preoperative evaluation conducted by our experienced orthopedic team. This assessment involves a detailed review of your medical history, a physical examination, and diagnostic imaging to evaluate the extent of damage to your hip joint. Our goal during this stage is to gain a comprehensive understanding of your condition and tailor a treatment plan that addresses your specific needs and goals.
Patient Education: We believe that informed patients make empowered decisions, which is why we prioritize patient education throughout the treatment process. Our team will provide you with detailed information about the hip replacement procedure, including what to expect before, during, and after surgery. We’ll discuss the different surgical approaches available, potential risks and complications, and strategies for optimizing your recovery. By arming you with knowledge and resources, we aim to ensure that you feel confident and prepared for your hip replacement journey.
State-of-the-Art Surgical Techniques: At Orthopedic Centers of Colorado, we utilize state-of-the-art surgical techniques and technologies to perform hip replacement procedures with the highest level of precision and safety. Our board-certified orthopedic surgeons have extensive experience in performing hip replacements and are committed to delivering exceptional outcomes for every patient. Whether you require a traditional total hip arthroplasty or a minimally invasive approach, our surgeons will tailor the procedure to meet your individual needs, ensuring optimal results and a faster recovery.
Postoperative Rehabilitation: Rehabilitation plays a crucial role in the success of your hip replacement surgery. Our team of rehabilitation specialists will work closely with you to develop a personalized rehabilitation plan aimed at optimizing your recovery and restoring function. This may include physical therapy exercises to improve strength and range of motion, as well as strategies for pain management and activities of daily living. We’ll provide you with the guidance and support you need to achieve the best possible outcome and regain independence.
Continued Follow-Up and Support: Our commitment to your well-being extends beyond surgery and rehabilitation. We’ll schedule regular follow-up appointments to monitor your progress, address any concerns or complications, and ensure that you’re on track to achieving your recovery goals. Our team is always available to answer questions, provide support, and adjust your treatment plan as needed to ensure your continued comfort and mobility.
Hip Procedures & Conditions Treated
We treat all hip injuries, below are a few of the more common conditions:
- Total Hip Replacement – Arthroplasty
- Arthritis
- Aspiration
- Avascular Necrosis
- Bursitis
- Cortisone Injections
- Decompression Surgery
- Denervation Procedures
- Dislocation & Dysplasia
- Distraction Arthroplasty
- Femoroacetabular Impingement
- Fracture
- Fusion – Arthrodesis
- Greater Trochanteric Pain Syndrome
- Hip Pointer
- Hip Resurfacing
- Labral Tears & Repair
- Nerve Block
- Osteoarthritis
- Osteotomy
- Piriformis Syndrome
- Revision Surgery
- Rheumatoid Arthritis
- Snapping Hip Syndrome
- Synovectomy
- Trochanteric Bursitis
- Tendon Repair
- Tendonitis
Patient-Centered Care
Our patient-centered approach is built on communication, collaboration, and compassion. We understand that every patient is unique, and we take the time to listen to your concerns, answer your questions, and involve you in decisions about your care. Our goal is not just to treat conditions but to empower you to lead an active, pain-free life.
Our dedicated team of healthcare professionals strives to create a compassionate and supportive environment where you feel heard, respected, and actively involved in your care decisions. Your health and satisfaction are our top priorities, and we are here to collaborate with you on a personalized care journey that respects your dignity and empowers you to achieve the best possible outcomes.

Hip Replacement & Arthritis Physicians
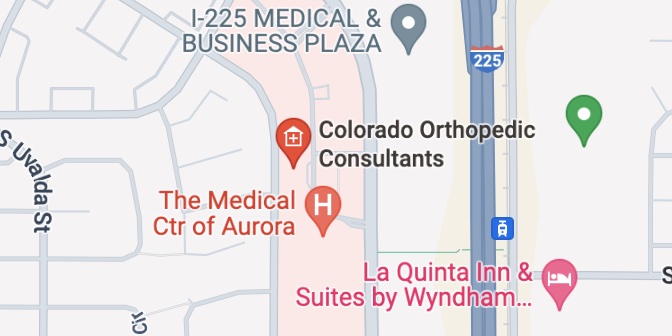
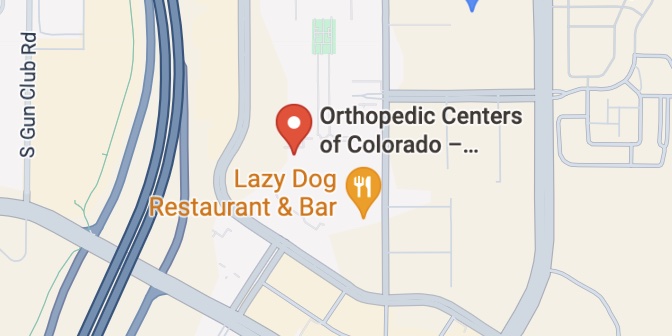
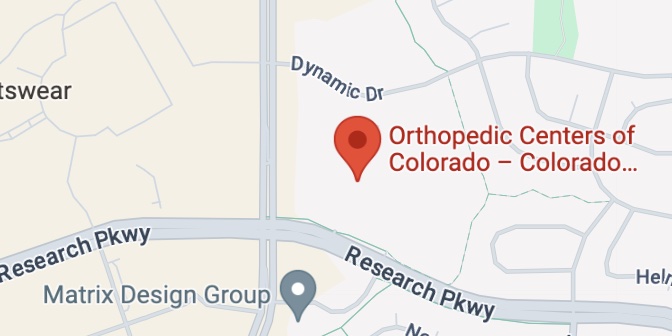
Hip Locations