Knee Replacement & Arthritis
Center of Excellence
At Orthopedic Centers of Colorado, we understand the impact that knee pain can have on your daily life. That’s why our team of expert orthopedic surgeons specializes in innovative knee replacement techniques designed to restore function and improve your quality of life.
Our personalized approach begins with a thorough evaluation to determine the best treatment plan for you. Whether you’re suffering from osteoarthritis, rheumatoid arthritis, or other knee conditions, we offer state-of-the-art knee replacement solutions tailored to your unique needs.
Schedule Now!
Click below to schedule
an appointment
Comprehensive Knee Care
Don’t let knee pain hold you back any longer. Take the first step toward a pain-free future by scheduling a consultation with our orthopedic specialists today. Together, we’ll help you reclaim your active lifestyle and get back to doing the things you love. Benefits of our orthopedic knee replacement services include:
Pain Relief: Say goodbye to debilitating knee pain and regain control of your life.
Improved Mobility: Rediscover the freedom to move comfortably and confidently.
Enhanced Functionality: Enjoy increased joint stability and functionality for everyday activities.
Long-Term Results: Our procedures are designed for lasting relief, allowing you to live your life to the fullest.
Expert Care: Trust in the expertise of our experienced orthopedic surgeons and dedicated medical team.
Knee Conditions & Procedures Treated
We treat all knee injuries, below are a few of the more common conditions:
- Total Knee Replacement:
Partial & Total - Acute Knee Injuries
- ACL – Anterior Cruciate Ligament Injuries
- Arthritis
- Arthroscopy
- Articular Cartilage Injuries
- Bursitis
- Cartilage Injuries
- Dislocations
- Fractures
- Ligament Injuries: PCL, MCL & LCL
- Meniscus Tears
- Muscle Injuries
- Osgood-Schlatter Disease
- Osteonecrosis
- Osteotomy
- Patellofemoral Injuries
- Runner’s Knee
- Tendinitis
Patient-Centered Care
Our patient-centered approach is built on communication, collaboration, and compassion. We understand that every patient is unique, and we take the time to listen to your concerns, answer your questions, and involve you in decisions about your care. Our goal is not just to treat conditions but to empower you to lead an active, pain-free life.
Our dedicated team of healthcare professionals strives to create a compassionate and supportive environment where you feel heard, respected, and actively involved in your care decisions. Your health and satisfaction are our top priorities, and we are here to collaborate with you on a personalized care journey that respects your dignity and empowers you to achieve the best possible outcomes.

Knee Replacement & Arthritis Physicians
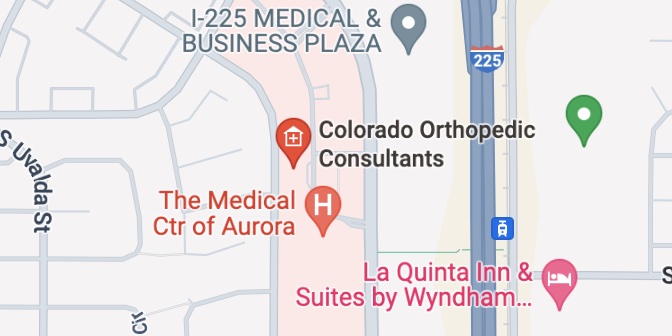
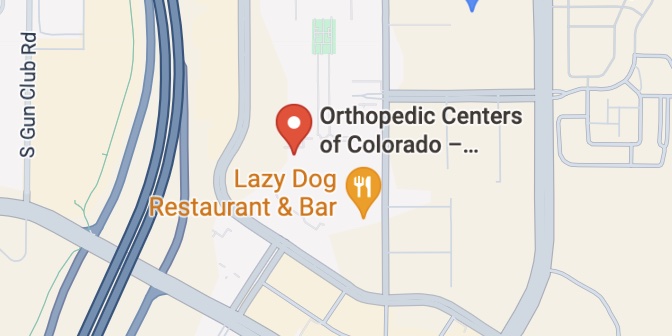
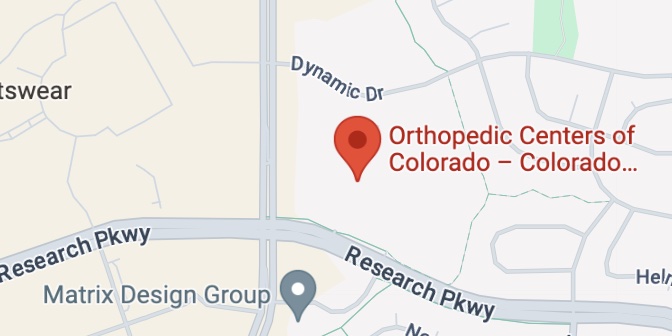
Knee Locations