Shoulder Replacement & Arthritis
Center of Excellence
At Orthopedic Centers of Colorado, we understand the profound impact shoulder pain and arthritis can have on your life. That’s why our board-certified physicians are dedicated to providing exceptional care and innovative solutions to help you regain mobility, reduce pain, and reclaim your quality of life.
We specialize in providing advanced care for shoulder replacement and arthritis management. Our dedicated team of orthopedic specialists focuses exclusively on addressing the unique needs of patients dealing with shoulder pain and arthritis, offering comprehensive solutions tailored to restore mobility and alleviate discomfort.
Schedule Now!
Click below to schedule
an appointment
Comprehensive Care
Specialized Expertise: Our center is staffed by a team of highly skilled orthopedic surgeons who specialize in shoulder replacement procedures. With years of experience and advanced training, they are dedicated to delivering the highest quality of care with precision and expertise.
Individualized Treatment Plans: We recognize that every patient is unique, which is why we take a personalized approach to your care. Our team will work closely with you to develop a tailored treatment plan that addresses your specific needs, preferences, and goals.
Advanced Surgical Techniques: We utilize the latest advancements in orthopedic surgery, including minimally invasive techniques and state-of-the-art prosthetic implants, to optimize surgical outcomes and promote faster recovery times.
Comprehensive Rehabilitation: Our care extends beyond the operating room. We offer comprehensive rehabilitation services, including physical therapy and occupational therapy, to help you regain strength, mobility, and function following surgery.
Ongoing Support: From your initial consultation through every step of your recovery journey, our compassionate team will be by your side, providing guidance, support, and encouragement to ensure your success.
Shoulder Procedures & Conditions Treated
We treat all shoulder injuries, below are a few of the more common conditions:
- Total Shoulder Replacement
- Acromioplasty
- Adhesive capsulitis – Frozen Shoulder
- Arthritis
- Arthroscopy
- Bankart Repair
- Biceps & Shoulder Tendonitis
- Bone Spurs
- Bursitis
- Capsular Release
- Cartilage Tear
- Dislocation, Separation & Instability
- Fractures
- Impingement Syndrome
- Labral Tear
- Osteoarthritis
- Rheumatoid Arthritis
- Rotator Cuff Tears & Repair
- SLAP Repair
- Shoulder Decompression
- Shoulder Impingement Syndrome
- Subacromial Decompression
- Tendinitis
Patient-Centered Care
Our patient-centered approach is built on communication, collaboration, and compassion. We understand that every patient is unique, and we take the time to listen to your concerns, answer your questions, and involve you in decisions about your care. Our goal is not just to treat conditions but to empower you to lead an active, pain-free life.
Our dedicated team of healthcare professionals strives to create a compassionate and supportive environment where you feel heard, respected, and actively involved in your care decisions. Your health and satisfaction are our top priorities, and we are here to collaborate with you on a personalized care journey that respects your dignity and empowers you to achieve the best possible outcomes.

Shoulder Replacement & Arthritis Physicians
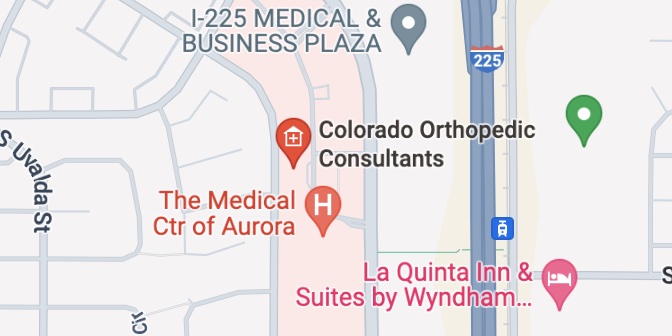
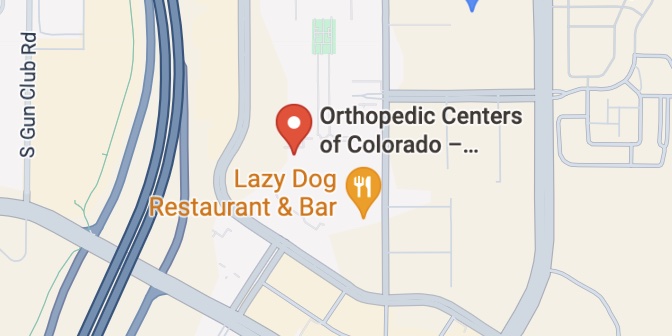
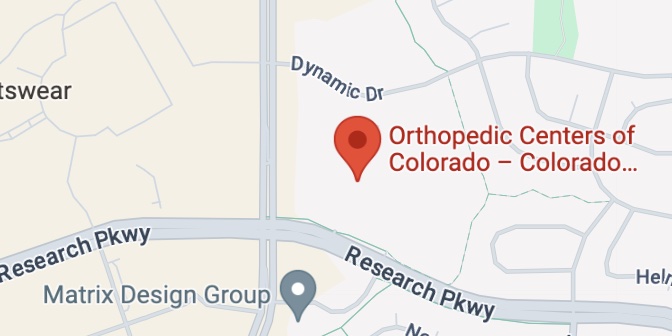
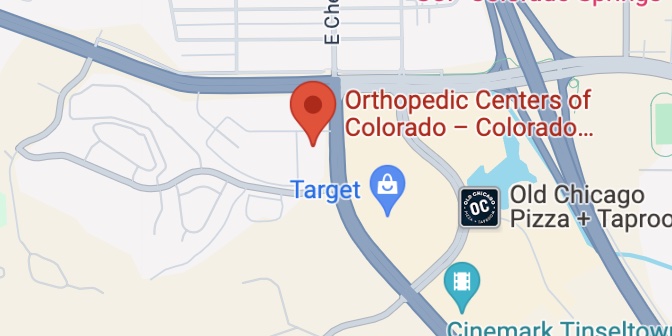
Shoulder Locations